Patellar syndrome: a mystery finally unraveled
Patellar syndrome is defined as a pain of a mechanical type felt in the anterior aspect of the knee. Compression moves such as squatting, climbing, descending stairs or prolonged sitting are factors that trigger or worsen the syndrome. Repetitive activities such as running cause the pain to flare up to the point that it is no longer practicable. The pain subsides with rest and is reversible, although it can persist for quite a long time after exercise, like the pain present in iliotibial band syndrome with which patellar syndrome may be associated.
Patellar syndrome predominantly affects a population that is often young, active or athletic, more female than male. In a specialist knee or sports medicine consultation, patellar syndrome alone accounts for 25 to 40% of the reasons for consultation.
The pain may be the only symptom or be associated with feelings of letting go or hooking up without it being patellar instability with apprehension of dislocation. The effusion is rare. The diagnosis is often made by exclusion, and radiological examinations usually show nothing abnormal – except sometimes transient edema of the patellar cartilage on an MRI scan. No correlation could be established between cartilage damage and pain, and the term patellar chondropathy is no longer used today to define this syndrome which does not progress to osteoarthritis.
Therapeutically, there is no real consensus. Many studies have been published which have shown encouraging results with comprehensive treatment based on stretching and sheathing. Plantar supports sometimes have a beneficial effect. Unfortunately, improvement is often transient and recurrence frequent. In the absence of regular training, the pains return and force patients to change their sports habits and lifestyles.
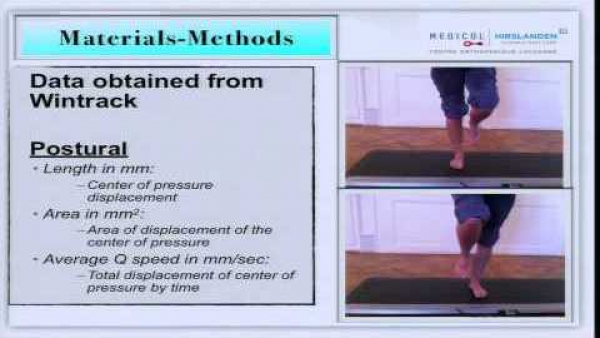
Patellar syndrome remains to this day a controversial subject without a valid explanation as to its etiology. Predisposing factors such as constitutional hyperlaxity or strong femoral antetorsion have been implicated, but this is a multifactorial problem. A functional disorder is at the origin of the syndrome and the explanation can only be found by analysis of movement.
The loss of physiological interarticular synchronism of walking is caused by a poorly understood and little researched clinical entity: Functional Hallux Limitus (FHL). In searching for it systematically for 20 years, I have found that this entity is present and can be diagnosed in all cases of patellar syndrome.

If we go back to the mapping of pain in patellar syndrome: unlike external hyper-pressure syndrome, the pain is antero-internal (medial) and appears during exertion, especially when running. The pain can be so violent that it forces people to stop the activity. If, subsequently, sport rest is observed, the pain will go away on its own. The explanation for this pain is the appearance of transient bone edema located on the inner side of the kneecap.
This is linked to the repetition of pressure and stresses that occur during the impact of the foot on the ground. Why? FHL causes desynchronization with gait which results in delayed quadriceps contraction when the foot lands on the ground. The patella at this precise moment is not applied to the outer side of the trochlea as it should be, but "floats" and is suddenly stuck on the inner side of the trochlea when the quadriceps contracts, too late. Patellar syndrome should be understood as a global dysfunction induced by FHL which happens on the patellofemoral.
Along with joint pain, pain can exist on the periphery of the knee, especially in the tendons. The most exposed are the iliotibial band (see pain syndrome of the iliotibial band or windshield wiper syndrome) and the crow's feet tendons located on the inner side of the tibial plateau. Why these tendons? Because they are attempting to combat the excessive external rotation of the tibia associated with excessive supination during the FHL-induced impact of the foot on the ground. The forces are particularly important since they are exerted in an eccentric mode (movement braking). Patients rarely complain of these pains but they are found consistently on palpation if we look for them.
Learn more
Knee: the patellofemoralClinical epidemiology and understanding of knee pain, a new approach to patellar syndrome
 Research: FHL and Gait Analysis
Research: FHL and Gait Analysis
 EN
EN  DE
DE  ES
ES  FR
FR 